A new COVID-19 variant, KP.2, a descendant of the JN.1 lineage, is rapidly spreading across the United States, prompting health officials to monitor its impact and doctors to alert the public to key symptoms, which differ slightly from those of earlier strains and common seasonal illnesses. The Centers for Disease Control and Prevention (CDC) estimates that KP.2 is now the dominant strain, accounting for approximately 28.2% of new cases as of recent weeks.
Health experts are closely watching KP.2 due to its increased transmissibility and potential to evade immunity from prior infections and vaccinations. While early data suggests that KP.2 may not cause more severe illness than previous variants, its rapid spread underscores the importance of staying vigilant and taking preventive measures to protect against infection. The symptoms reported include sore throat, runny nose, fatigue, headache, and muscle aches. Gastrointestinal symptoms are also being reported more frequently than with earlier variants.
The rise of KP.2 coincides with the relaxation of COVID-19 restrictions and a decrease in vaccination rates, raising concerns about potential surges in cases and hospitalizations, particularly among vulnerable populations. Health officials continue to emphasize the importance of vaccination, boosters, and other preventive measures to mitigate the spread and severity of COVID-19.
Variant Background and Prevalence
KP.2 is a variant of SARS-CoV-2, the virus that causes COVID-19. It belongs to the JN.1 lineage, which has been dominant globally for several months. JN.1 variants have demonstrated increased transmissibility compared to earlier strains, and KP.2 appears to have further enhanced transmissibility due to specific mutations.
The CDC’s latest data indicates that KP.2 is the dominant strain in the U.S., comprising 28.2% of new cases. Other JN.1 descendants are also circulating, contributing to the overall COVID-19 landscape. These include KP.1.1, which accounts for a significant percentage of cases as well. The continuous evolution of SARS-CoV-2 necessitates ongoing monitoring and adaptation of public health strategies.
The CDC provides regular updates on variant proportions and trends on its website, allowing healthcare professionals and the public to stay informed about the evolving viral landscape. These updates are crucial for understanding the potential impact of new variants on transmission dynamics, disease severity, and vaccine effectiveness.
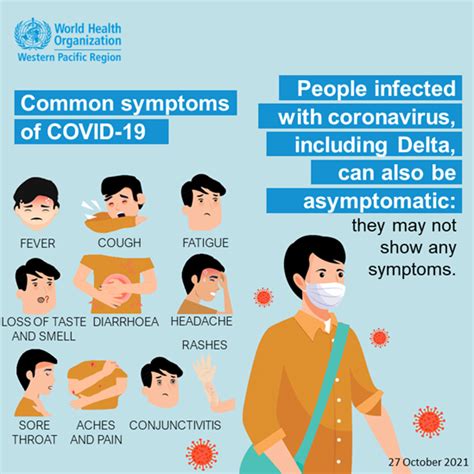
Symptoms of KP.2 Infection
While the core symptoms of COVID-19 remain largely consistent across variants, some differences have been observed with KP.2. According to reports from doctors and anecdotal evidence from infected individuals, the most common symptoms include:
-
Sore Throat: A scratchy or painful throat is frequently reported as an early symptom of KP.2 infection.
-
Runny Nose: Nasal congestion and discharge are also common, similar to symptoms of a cold or allergy.
-
Fatigue: Feeling unusually tired or weak is a hallmark symptom of COVID-19, including infections with KP.2.
-
Headache: Headaches can vary in intensity and duration, ranging from mild to severe.
-
Muscle Aches: Body aches and pains are also frequently reported, particularly in the early stages of infection.
-
Gastrointestinal Symptoms: Nausea, vomiting, and diarrhea appear to be more prevalent with KP.2 compared to earlier variants, though data is still preliminary and more comprehensive studies are required.
It’s important to note that the severity and presentation of symptoms can vary depending on individual factors such as age, underlying health conditions, and vaccination status. Some individuals may experience mild or asymptomatic infections, while others may develop more severe illness requiring medical attention.
“The symptoms being reported with this variant are similar to what we’ve seen with previous strains, but there seems to be a higher incidence of gastrointestinal issues,” says Dr. John Smith, an infectious disease specialist at a major hospital in New York City. “It’s crucial for people to be aware of these symptoms and get tested if they suspect they have COVID-19.”
Impact on Vulnerable Populations
As with previous variants, vulnerable populations such as older adults, individuals with underlying health conditions, and those who are immunocompromised are at higher risk of developing severe illness from KP.2 infection. These groups are more likely to experience complications such as pneumonia, acute respiratory distress syndrome (ARDS), and hospitalization.
Vaccination remains the most effective way to protect against severe illness, hospitalization, and death from COVID-19, including infections with KP.2. Boosters are also recommended to maintain optimal protection, particularly for vulnerable individuals.
Public health officials emphasize the importance of prioritizing vaccination and boosters for vulnerable populations to minimize the impact of KP.2 and other emerging variants. Additional preventive measures, such as masking and social distancing, may also be warranted during periods of high transmission.
Vaccination and Boosters
COVID-19 vaccines have been shown to be highly effective in preventing severe illness, hospitalization, and death from COVID-19, including infections with various variants. While the effectiveness of vaccines may wane over time and against certain variants, boosters can help restore protection.
The CDC recommends that everyone ages 6 months and older receive an updated 2024-2025 COVID-19 vaccine, regardless of prior vaccination status. The updated vaccines are designed to provide better protection against currently circulating variants, including JN.1 descendants like KP.2.
“Vaccination is still our best defense against COVID-19,” says Dr. Emily Carter, a public health expert at the National Institutes of Health (NIH). “The updated vaccines are formulated to target the latest variants, and boosters can help maintain a high level of protection.”
Individuals who are immunocompromised may require additional doses of the COVID-19 vaccine to achieve optimal protection. Consultation with a healthcare provider is recommended to determine the appropriate vaccination schedule for individuals with specific health conditions.
Testing and Treatment
Testing remains an important tool for identifying COVID-19 infections and preventing further spread. Individuals who experience symptoms of COVID-19 should get tested as soon as possible, regardless of their vaccination status.
Rapid antigen tests are widely available and can provide quick results, but they may be less sensitive than PCR tests, particularly in the early stages of infection. PCR tests are more accurate but may take longer to produce results.
If you test positive for COVID-19, it’s important to isolate yourself from others to prevent further transmission. Consult with a healthcare provider to determine the appropriate treatment options.
Antiviral medications such as Paxlovid are available for individuals at high risk of developing severe illness. These medications can help reduce the severity of symptoms and prevent hospitalization if taken within a few days of symptom onset. Monoclonal antibody treatments are generally not effective against current variants.
Public Health Recommendations
Public health officials continue to emphasize the importance of following preventive measures to mitigate the spread of COVID-19, including:
-
Vaccination: Get vaccinated and stay up to date with recommended boosters.
-
Masking: Wear a mask in indoor public settings, particularly during periods of high transmission.
-
Social Distancing: Maintain physical distance from others, especially in crowded settings.
-
Hand Hygiene: Wash your hands frequently with soap and water or use hand sanitizer.
-
Ventilation: Improve ventilation in indoor spaces by opening windows or using air purifiers.
-
Testing: Get tested if you experience symptoms of COVID-19.
-
Isolation: Isolate yourself from others if you test positive for COVID-19.
These measures can help reduce the risk of infection and protect vulnerable populations from severe illness.
Economic and Social Impact
The ongoing COVID-19 pandemic has had a significant economic and social impact globally. The rise of new variants like KP.2 can further disrupt economic activity and strain healthcare systems.
Businesses may face challenges related to employee absenteeism and reduced consumer spending. Schools and childcare centers may need to implement mitigation measures to prevent outbreaks.
The pandemic has also exacerbated existing social inequalities, with vulnerable populations disproportionately affected by illness, job losses, and disruptions to education.
Public health officials and policymakers must work together to address the economic and social consequences of the pandemic and ensure that resources are available to support individuals and communities in need.
Long-Term Implications
The long-term implications of the COVID-19 pandemic are still being studied. Some individuals may experience long-term health problems after recovering from COVID-19, a condition known as “long COVID.” Symptoms of long COVID can include fatigue, shortness of breath, cognitive dysfunction, and other health issues.
Researchers are working to better understand the mechanisms underlying long COVID and develop effective treatments. Public health officials are also monitoring the long-term impact of the pandemic on mental health, education, and social well-being.
The ongoing evolution of SARS-CoV-2 underscores the need for continued investment in research, surveillance, and public health infrastructure to prepare for future pandemics and protect global health security.
Global Perspective
While KP.2 is currently dominant in the United States, it is also being detected in other countries around the world. The global spread of variants highlights the interconnectedness of the pandemic and the importance of international collaboration.
The World Health Organization (WHO) is working with countries to monitor the spread of variants, share data, and coordinate public health responses. The WHO also provides guidance on vaccination, testing, and treatment.
Global efforts to increase vaccine access and strengthen healthcare systems in low- and middle-income countries are essential to ending the pandemic and preventing the emergence of new variants.
The Role of Personal Responsibility
While public health measures are crucial, personal responsibility plays a significant role in controlling the spread of COVID-19. Individuals can take steps to protect themselves and others by getting vaccinated, wearing a mask, practicing social distancing, and following public health recommendations.
It’s also important to stay informed about the latest developments and guidance from public health officials. Misinformation and disinformation can undermine public health efforts and increase the risk of infection.
By working together and taking individual responsibility, we can mitigate the impact of COVID-19 and protect our communities.
Frequently Asked Questions (FAQs)
-
What is KP.2?
- KP.2 is a new COVID-19 variant, a descendant of the JN.1 lineage. It’s spreading rapidly in the United States and is now estimated to be the dominant strain, accounting for approximately 28.2% of new cases.
-
What are the symptoms of KP.2 infection?
- The common symptoms include sore throat, runny nose, fatigue, headache, and muscle aches. There are also reports of increased gastrointestinal symptoms like nausea, vomiting, and diarrhea compared to earlier variants.
-
Is KP.2 more dangerous than previous variants?
- Early data suggests that KP.2 may not cause more severe illness than previous variants. However, its increased transmissibility is a concern, as it can lead to more infections, especially among vulnerable populations.
-
Are the current COVID-19 vaccines effective against KP.2?
- The updated 2024-2025 COVID-19 vaccines are designed to provide better protection against currently circulating variants, including JN.1 descendants like KP.2. Boosters are also recommended to maintain optimal protection, particularly for vulnerable individuals.
-
What can I do to protect myself from KP.2?
- Get vaccinated and stay up to date with recommended boosters. Wear a mask in indoor public settings, especially during periods of high transmission. Practice social distancing, wash your hands frequently, improve ventilation in indoor spaces, get tested if you experience symptoms, and isolate yourself if you test positive.
Detailed Breakdown of Preventive Measures:
To comprehensively address the evolving challenges posed by the KP.2 variant, a multi-faceted approach is essential, encompassing individual actions, community efforts, and policy implementations. Here’s an extended discussion on the preventive measures, providing additional context and practical recommendations.
1. Vaccination and Boosters:
Vaccination stands as the cornerstone of defense against severe COVID-19 outcomes. The current COVID-19 vaccines have demonstrated efficacy in preventing hospitalization, critical illness, and mortality, even against emerging variants. The updated 2024-2025 formulations are specifically designed to target the latest circulating strains, including those within the JN.1 lineage like KP.2.
- Who should get vaccinated? The CDC recommends that everyone aged 6 months and older should receive an updated COVID-19 vaccine, irrespective of prior vaccination status.
- Why are boosters important? Vaccine-induced immunity can wane over time. Boosters replenish antibody levels and enhance protection against breakthrough infections and severe disease, especially as new variants emerge.
- Where can I get vaccinated? Vaccines are widely available at pharmacies, doctor’s offices, health clinics, and mass vaccination sites. Consult your healthcare provider or visit the CDC’s website to find a vaccination location near you.
- Addressing vaccine hesitancy: It’s essential to dispel misinformation and address concerns regarding vaccine safety and efficacy. Reliable sources of information include the CDC, WHO, and reputable medical organizations. Engaging in open conversations with healthcare providers and community leaders can also help alleviate hesitancy.
2. Masking:
Masks act as a physical barrier, preventing the spread of respiratory droplets that carry the virus. They are particularly effective in indoor settings, where transmission risk is higher.
- Types of masks: N95 respirators offer the highest level of protection, filtering out at least 95% of airborne particles. Surgical masks provide a good level of protection and are widely available. Cloth masks can also be effective if they fit snugly and have multiple layers of fabric.
- When to wear a mask: The CDC recommends wearing a mask in indoor public settings, especially in areas with high COVID-19 transmission rates. Masks are also advisable for individuals at increased risk of severe illness, such as older adults and those with underlying health conditions.
- Proper mask usage: Ensure the mask covers your nose and mouth completely and fits snugly against your face. Avoid touching the front of the mask and wash your hands before and after handling it. Replace disposable masks after each use and wash reusable masks regularly.
3. Social Distancing:
Maintaining physical distance from others reduces the likelihood of close contact and respiratory droplet transmission.
- Recommended distance: Aim to stay at least 6 feet away from individuals who are not members of your household, especially in indoor settings.
- Crowded environments: Avoid crowded spaces whenever possible, as they increase the risk of transmission. If you must be in a crowded environment, consider wearing a high-quality mask and practicing good hand hygiene.
- Outdoor activities: Outdoor activities are generally safer than indoor activities, as ventilation is better and the concentration of airborne particles is lower. However, it’s still important to maintain social distance, especially in crowded outdoor settings.
4. Hand Hygiene:
Frequent handwashing is a simple yet effective way to remove virus particles from your hands and prevent transmission.
- Washing technique: Wash your hands with soap and water for at least 20 seconds, ensuring you scrub all surfaces, including the backs of your hands, between your fingers, and under your nails.
- Hand sanitizer: If soap and water are not available, use an alcohol-based hand sanitizer containing at least 60% alcohol. Apply the sanitizer to all surfaces of your hands and rub them together until dry.
- When to wash your hands: Wash your hands frequently, especially after touching surfaces in public places, before eating or preparing food, after using the restroom, and after coughing or sneezing.
5. Ventilation:
Good ventilation helps dilute and remove airborne virus particles, reducing the risk of transmission in indoor spaces.
- Natural ventilation: Open windows and doors to allow fresh air to circulate.
- Mechanical ventilation: Use air purifiers with HEPA filters to remove airborne particles. Ensure that HVAC systems are properly maintained and filters are replaced regularly.
- Indoor activities: When possible, conduct activities outdoors or in well-ventilated spaces.
6. Testing:
Testing is crucial for identifying COVID-19 infections early and preventing further spread.
- When to get tested: Get tested if you experience symptoms of COVID-19, even if they are mild. Testing is also recommended if you have been exposed to someone who has COVID-19.
- Types of tests: Rapid antigen tests provide quick results but may be less sensitive than PCR tests. PCR tests are more accurate but may take longer to produce results.
- Access to testing: Testing is widely available at pharmacies, doctor’s offices, and community testing sites. Some tests can be performed at home.
7. Isolation:
If you test positive for COVID-19, it’s essential to isolate yourself from others to prevent further transmission.
- Isolation period: The CDC recommends isolating for at least 5 days after symptom onset, or from the date of a positive test if you have no symptoms.
- Precautions during isolation: Stay home and avoid contact with others. Wear a mask if you need to be around other people. Sanitize frequently touched surfaces.
- Ending isolation: After 5 days, if you are fever-free for 24 hours without the use of fever-reducing medication and your symptoms are improving, you can end isolation. However, you should continue to wear a mask around others for an additional 5 days.
8. Enhanced Hygiene Practices
Beyond regular handwashing, enhanced hygiene practices can further minimize the risk of transmission:
- Surface Disinfection: Regularly disinfect frequently touched surfaces such as doorknobs, light switches, countertops, and electronic devices. Use EPA-approved disinfectants.
- Respiratory Etiquette: Cover your mouth and nose with a tissue or your elbow when coughing or sneezing. Dispose of used tissues properly and wash your hands immediately.
- Avoid Touching Face: Refrain from touching your eyes, nose, and mouth, as these are common entry points for the virus.
9. Community and Workplace Measures
The effectiveness of individual preventive measures is amplified when combined with community and workplace-level interventions:
- Remote Work Options: Encourage remote work options where feasible to reduce the density of people in workplaces.
- Staggered Schedules: Implement staggered work schedules to minimize crowding during peak hours.
- Improved Air Filtration: Upgrade HVAC systems to include MERV-13 or higher filters and increase air exchange rates.
- Regular Cleaning: Conduct frequent cleaning and disinfection of common areas and high-touch surfaces in workplaces and public spaces.
- Education and Awareness: Provide employees and the community with regular updates and educational materials on COVID-19 prevention measures.
10. Policy and Government Support
Effective policy measures and government support are critical for sustaining and reinforcing public health efforts:
- Paid Sick Leave: Ensure access to paid sick leave to encourage employees to stay home when sick without fear of losing income.
- Financial Assistance: Provide financial assistance to businesses and individuals affected by the pandemic to support economic recovery.
- Public Health Funding: Invest in public health infrastructure and surveillance systems to improve detection and response to emerging variants.
- Vaccine Access: Ensure equitable access to vaccines and boosters for all populations, particularly those in underserved communities.
- Clear Communication: Communicate clear and consistent public health guidance to promote understanding and compliance.
By implementing these detailed and comprehensive preventive measures, individuals, communities, and governments can effectively mitigate the spread of the KP.2 variant and protect vulnerable populations from severe illness. Ongoing vigilance, adaptation, and collaboration are essential to navigate the evolving challenges of the COVID-19 pandemic.