A new, highly transmissible COVID-19 variant, KP.2, a descendant of the JN.1 lineage, is rapidly spreading across the United States, raising concerns among health officials. This variant, now estimated to be responsible for a significant proportion of new COVID-19 cases, exhibits increased transmissibility compared to previous strains, though current evidence suggests it does not cause more severe illness. Experts emphasize the importance of staying vigilant, recognizing potential symptoms, and utilizing available preventative measures, including vaccination and booster shots.
The rise of KP.2 underscores the virus’s continued evolution and ability to adapt, highlighting the need for ongoing monitoring and public health preparedness. While scientists are still gathering data on this new variant, early observations indicate that its mutations may allow it to evade existing immunity more effectively. The Centers for Disease Control and Prevention (CDC) is closely tracking KP.2 and providing updated guidance to healthcare providers and the public.
KP.2: What We Know So Far
KP.2 is a sub-lineage of JN.1, which was the dominant variant earlier this year. As the virus evolves, new variants and sub-variants emerge, each with unique characteristics that can affect their transmissibility, severity, and ability to evade immune responses. KP.2 appears to have gained a foothold due to its increased transmissibility, allowing it to outcompete other circulating variants.
“It’s not surprising to see new variants emerge,” explains Dr. Peter Hotez, a vaccine scientist at Baylor College of Medicine. “The virus is constantly mutating, and some mutations can make it more contagious.”
The emergence of KP.2 serves as a reminder that the COVID-19 pandemic is not over and that continued vigilance is essential. Although vaccines and boosters offer protection against severe illness, new variants can still cause breakthrough infections, particularly in individuals who are immunocompromised or have underlying health conditions.
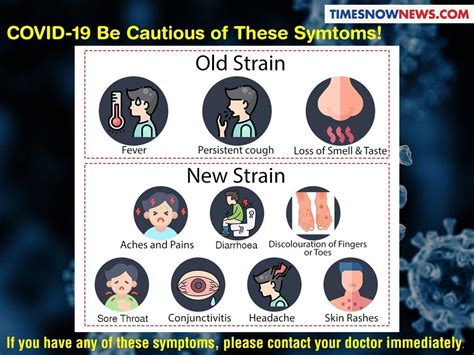
Signs and Symptoms to Watch For
The symptoms associated with KP.2 are generally similar to those of previous COVID-19 variants, including:
- Fever or chills
- Cough
- Sore throat
- Congestion or runny nose
- Muscle or body aches
- Headache
- Fatigue
- Shortness of breath or difficulty breathing
- New loss of taste or smell
- Nausea or vomiting
- Diarrhea
It is important to note that not everyone infected with KP.2 will experience all of these symptoms, and some individuals may be asymptomatic. The severity of symptoms can also vary depending on individual factors such as age, underlying health conditions, and vaccination status.
If you experience any of these symptoms, it is recommended to get tested for COVID-19 and consult with a healthcare provider. Early diagnosis and treatment can help prevent severe illness and reduce the risk of transmission to others.
Transmission and Prevention
KP.2 spreads through respiratory droplets produced when an infected person coughs, sneezes, talks, or breathes. The virus can be transmitted through close contact with an infected person or by touching a contaminated surface and then touching your face.
The following preventative measures can help reduce the risk of infection with KP.2 and other COVID-19 variants:
- Get vaccinated and boosted: Vaccines and boosters are highly effective in preventing severe illness, hospitalization, and death from COVID-19.
- Wear a mask: Wearing a well-fitting mask in public indoor settings can help reduce the spread of respiratory droplets.
- Practice good hygiene: Wash your hands frequently with soap and water for at least 20 seconds, or use an alcohol-based hand sanitizer.
- Maintain social distancing: Avoid close contact with people who are sick, and maintain a distance of at least six feet from others in public settings.
- Ventilate indoor spaces: Open windows and doors to improve ventilation and reduce the concentration of viral particles in the air.
- Stay home if you are sick: If you experience symptoms of COVID-19, stay home and avoid contact with others.
- Get tested: If you have been exposed to COVID-19 or are experiencing symptoms, get tested to determine if you are infected.
The Importance of Vaccination
Vaccination remains the most effective tool in preventing severe illness and hospitalization from COVID-19. While vaccines may not completely prevent infection, they significantly reduce the risk of serious complications.
“Vaccines are still highly effective in preventing severe illness, even against new variants,” says Dr. Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases. “It’s important for people to stay up to date on their vaccinations, including booster shots.”
The CDC recommends that everyone ages 6 months and older receive an updated 2024-2025 COVID-19 vaccine, regardless of prior vaccination status. The updated vaccines are designed to provide better protection against current circulating variants.
Treatment Options
Several treatment options are available for individuals who test positive for COVID-19, including:
- Antiviral medications: Antiviral medications such as Paxlovid can help reduce the severity of symptoms and prevent hospitalization, especially when taken early in the course of the illness.
- Monoclonal antibodies: Monoclonal antibodies are another type of treatment that can help neutralize the virus and prevent severe illness. However, some monoclonal antibody treatments may be less effective against certain variants.
- Supportive care: Supportive care includes rest, fluids, and over-the-counter medications to relieve symptoms such as fever, cough, and pain.
It is important to consult with a healthcare provider to determine the best treatment option for your individual situation.
The Future of COVID-19
The emergence of KP.2 and other new variants underscores the ongoing evolution of the COVID-19 virus and the need for continued vigilance. Scientists are constantly monitoring the virus and developing new vaccines and treatments to combat its spread.
“We need to be prepared for the possibility of new variants emerging in the future,” says Dr. Rochelle Walensky, former director of the CDC. “Continued investment in research and development is essential to stay ahead of the virus.”
While the COVID-19 pandemic has presented numerous challenges, it has also spurred significant advances in science and medicine. The development of mRNA vaccines, for example, has revolutionized vaccine technology and has the potential to be used to combat other infectious diseases.
Long-Term Effects of COVID-19
In addition to the acute symptoms of COVID-19, some individuals may experience long-term effects, known as long COVID. Long COVID can manifest in a variety of ways, including fatigue, shortness of breath, cognitive dysfunction, and chronic pain.
The exact causes of long COVID are still being investigated, but it is believed to be related to persistent inflammation, immune dysregulation, and damage to organs and tissues.
If you are experiencing long-term effects after a COVID-19 infection, it is important to seek medical care. There are specialized clinics and healthcare providers who can help manage the symptoms of long COVID and improve quality of life.
Global Impact
The COVID-19 pandemic has had a profound impact on the world, affecting economies, healthcare systems, and social structures. The pandemic has also exacerbated existing inequalities, with vulnerable populations disproportionately affected.
Global cooperation is essential to combat the pandemic and ensure equitable access to vaccines and treatments. International organizations such as the World Health Organization (WHO) play a critical role in coordinating the global response to COVID-19.
Public Health Recommendations
Public health officials continue to emphasize the importance of following public health recommendations to protect yourself and others from COVID-19. These recommendations include:
- Get vaccinated and boosted: Vaccines and boosters are the best way to protect yourself from severe illness and hospitalization.
- Wear a mask: Wear a well-fitting mask in public indoor settings, especially when transmission rates are high.
- Practice good hygiene: Wash your hands frequently with soap and water, or use an alcohol-based hand sanitizer.
- Maintain social distancing: Avoid close contact with people who are sick, and maintain a distance of at least six feet from others in public settings.
- Ventilate indoor spaces: Open windows and doors to improve ventilation and reduce the concentration of viral particles in the air.
- Stay home if you are sick: If you experience symptoms of COVID-19, stay home and avoid contact with others.
- Get tested: If you have been exposed to COVID-19 or are experiencing symptoms, get tested to determine if you are infected.
By following these recommendations, we can all help to reduce the spread of COVID-19 and protect our communities.
Economic Impact
The COVID-19 pandemic has had a significant economic impact, causing widespread job losses, business closures, and disruptions to global supply chains. The pandemic has also led to increased government spending on healthcare, unemployment benefits, and economic stimulus programs.
The economic recovery from the pandemic is expected to be gradual and uneven, with some sectors recovering more quickly than others. The long-term economic consequences of the pandemic are still being assessed.
Mental Health
The COVID-19 pandemic has also taken a toll on mental health, with many people experiencing increased stress, anxiety, and depression. The pandemic has also led to increased social isolation and loneliness.
If you are struggling with your mental health, it is important to seek help. There are many resources available to support mental health, including therapy, counseling, and support groups.
Addressing Misinformation
Misinformation and disinformation about COVID-19 have been widespread throughout the pandemic, undermining public health efforts and contributing to vaccine hesitancy. It is important to rely on credible sources of information, such as the CDC and WHO, to make informed decisions about your health.
Social media companies have a responsibility to combat the spread of misinformation on their platforms. Fact-checking organizations and journalists play a critical role in debunking false claims and providing accurate information to the public.
The Role of Technology
Technology has played a crucial role in the response to the COVID-19 pandemic. Telemedicine has allowed healthcare providers to provide care remotely, reducing the risk of transmission. Contact tracing apps have helped to identify and isolate infected individuals. Data analytics have been used to track the spread of the virus and inform public health interventions.
Technology will continue to play an important role in the ongoing fight against COVID-19 and other infectious diseases.
Moving Forward
The COVID-19 pandemic has been a challenging time for everyone, but it has also demonstrated our resilience and ability to adapt. By working together and following public health recommendations, we can overcome the challenges of the pandemic and build a healthier and more resilient future. Continued research, innovation, and global cooperation are essential to ensure that we are prepared for future pandemics.
The focus must remain on protecting the most vulnerable members of our communities, ensuring equitable access to healthcare, and addressing the long-term consequences of the pandemic. The lessons learned from the COVID-19 pandemic will help us to better prepare for and respond to future public health emergencies.
The rise of KP.2 is a reminder that the fight against COVID-19 is not over. Vigilance, vaccination, and adherence to public health guidelines remain crucial to protecting ourselves and our communities. Staying informed and adapting to the evolving nature of the virus are essential for navigating the ongoing pandemic.
FAQ: KP.2 Variant
Q1: What is the KP.2 variant and why is it concerning?
A1: KP.2 is a sub-lineage of the JN.1 variant of COVID-19. It’s concerning because it appears to be more transmissible than previous strains, allowing it to spread more quickly. While current evidence doesn’t indicate it causes more severe illness, increased transmission can still lead to a rise in cases and potential strain on healthcare systems. “It’s not surprising to see new variants emerge,” explains Dr. Peter Hotez, a vaccine scientist at Baylor College of Medicine. “The virus is constantly mutating, and some mutations can make it more contagious.”
Q2: What are the symptoms of KP.2? Are they different from previous COVID-19 variants?
A2: The symptoms of KP.2 are generally similar to those of other COVID-19 variants. Common symptoms include fever or chills, cough, sore throat, congestion or runny nose, muscle or body aches, headache, fatigue, shortness of breath or difficulty breathing, new loss of taste or smell, nausea or vomiting, and diarrhea. There is no evidence to suggest that KP.2 causes significantly different symptoms.
Q3: How can I protect myself from the KP.2 variant? Are the current vaccines effective?
A3: The best way to protect yourself from KP.2 is to get vaccinated and boosted with the updated 2024-2025 COVID-19 vaccine. Vaccines remain highly effective in preventing severe illness, hospitalization, and death, even against new variants. In addition to vaccination, practicing good hygiene, wearing a mask in public indoor settings, maintaining social distancing, and ventilating indoor spaces can help reduce the risk of infection. “Vaccines are still highly effective in preventing severe illness, even against new variants,” says Dr. Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases. “It’s important for people to stay up to date on their vaccinations, including booster shots.”
Q4: If I test positive for COVID-19, what treatment options are available?
A4: Several treatment options are available, including antiviral medications like Paxlovid, which can help reduce the severity of symptoms and prevent hospitalization, especially when taken early. Monoclonal antibody treatments may also be an option, although their effectiveness can vary against different variants. Supportive care, including rest, fluids, and over-the-counter medications, can help relieve symptoms. It is important to consult with a healthcare provider to determine the best treatment plan for your individual situation.
Q5: What is the CDC doing to monitor the KP.2 variant? What should I do if I think I have KP.2?
A5: The CDC is closely tracking KP.2 and providing updated guidance to healthcare providers and the public. They monitor the prevalence of different variants, assess their characteristics, and provide recommendations for prevention and treatment. If you experience symptoms of COVID-19, it is recommended to get tested and consult with a healthcare provider. Early diagnosis and treatment can help prevent severe illness and reduce the risk of transmission to others. Public health officials continue to emphasize the importance of following public health recommendations to protect yourself and others from COVID-19. These recommendations include vaccination, masking, good hygiene, social distancing, and ventilation.